More and more often bacterial infections cannot be treated because antibiotics are no longer effective. The consequence is antibiotic resistance of the sick people. Why this is a problem and what role multi-resistant germs play.
 © iStock.com/alphaspirit
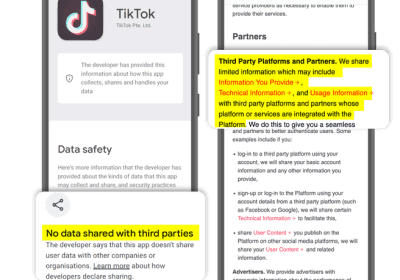
© iStock.com/alphaspiritOne of the most common causes of antibiotic resistance is that too many antibiotics are routinely used around the world. In many countries, the drugs are available without a prescription. In agriculture, too, animals receive massive amounts of antibiotics, mostly as a preventive measure against diseases – the residues then end up in the food chain. The careless and improper use of antibiotics mean that new resistances are constantly developing.
What is antibiotic resistance?
Antibiotics are among the most important medical discoveries. Doctors use them for bacterial infections. These active ingredients prevent bacteria from multiplying and kill them. For example, they help with life-threatening diseases such as pneumonia and are also an important weapon against hospital germs. A well-known antibiotic is penicillin , which the bacteriologist Alexander Fleming discovered in 1928. Other well-known antibiotics are aureomycin, chloramphenicol, streptomycin and tetracycline. An economical and targeted use of antibiotics is important in order to maintain their effectiveness.
In recent years, more and more bacteria have developed resistance to antibiotics. In the case of resistance, a type of bacteria is able to protect itself against a certain antibiotic. As a result, the drug loses its effectiveness.
Multi-resistant super germs
If a bacterium is able to protect itself against several antibiotics, scientists speak of a multi-resistant pathogen. The more often different antibiotics are taken, the higher the risk that (multi) resistant bacteria will develop and spread.
Numerous types of bacteria, against which antibiotics are no longer effective today, could previously be effectively combated. But every now and then a bacterium changes its genetic makeup. These genetic changes create new characteristics – and it may acquire resistance. As a result, these bacteria survive the use of a certain antibiotic and can continue to multiply without hindrance. They can even transfer this property from one type of bacteria to another.
One of the reasons for antibiotic resistance is that many people take the drugs too often and improperly. It is therefore important that we only take antibiotics when it is really necessary. What you need to know:
- Antibiotics only work against bacteria. It makes sense to use an antibiotic in the case of a severe bacterial infection, such as pneumonia or meningitis.
- Antibiotics don’t work for viral infections. Respiratory illnesses such as coughs , runny nose , flu , acute otitis media and bronchitis are usually caused by viruses. They cannot be treated with antibiotics if the disease progresses normally.
- It is important to take the medication exactly as the doctor prescribed. Only then can the antibiotic develop its effect.
Animal husbandry and antibiotic resistance are related
Bacteria that carry the resistance information spread through various channels: the frequent use of antibiotics in animal husbandry, for example, encourages resistant bacteria to develop and also be transmitted to humans – for example through the consumption of meat contaminated with bacteria or through direct contact with animals. In addition, drug residues find their way into the soil via the manure, which can lead to the development of resistant germs. Crop plants that are on our menu take up these germs as they grow – and we ingest them with our food.
What are the consequences of antibiotic resistance?
Antibiotic resistance is particularly problematic in poorer countries. Because an infection with a resistant bacterium is usually difficult or impossible to cure. Newer effective drugs are usually very expensive because they are not yet mass-produced – and their development takes a long time. The first new resistances often develop shortly after the market launch. In many cases, however, there is no remedy at all against the pathogen. If resistance spreads and researchers fail to discover effective new drugs, we are threatened with the risk of a child, for example, dying again from a simple bacterial disease that could have been cured earlier.
The negative consequences at a glance:
- Infections last longer
- Bacterial infections are more difficult to treat
- There are currently no effective antibiotics for some infections
- Originally easily treatable infections become life-threatening due to the resistance
- Multi-resistant pathogens (MRE) develop
Which bacteria are resistant so far?
Various types of bacteria are already resistant to antibiotics. They include:
- Enterococci
- Staphylococci (for example the methicillin-resistant Staphylococcus aureus, MRSA for short)
Other genera have also developed resistant strains. They include:
- Escherichia coli
- Klebsiella
- Pseudomonads
How dangerous are multi-resistant germs?
The emergence of (multi) resistant germs is a big problem. Especially in hospitals and other health facilities where antibiotics are administered. The consequences are life-threatening pneumonia as well as wound and blood infections. Young children as well as older and chronically ill people are particularly at risk.
Simple measures help prevent antibiotic resistance
In 2015, the Federal Ministry of Health worked together with the Federal Ministries of Food and Agriculture as well as Education and Research to develop the German antibiotic resistance strategy “DART 2020”. But you can also do something yourself:
- Only take antibiotics when you really need to. In this way you reduce the risk of developing resistance.
- Take an antibiotic for as long as the doctor tells you. Also note the correct dosage and the prescribed intake time.
- Do not give leftover antibiotics to others on your own, even if the symptoms are similar.
- Do not throw old medication or drug residues down the toilet or down the sink drain. This damages the environment and can contribute to the formation of resistances, as these enter the water cycle directly. Put old medicines in the trash.
- Try over-the-counter medicines and home remedies for a sore throat , runny nose, and other simple respiratory problems .
How to Avoid Infections
Avoid infections through simple hygiene measures:
- Wash your hands regularly and thoroughly.
- Avoid touching your face with your hands if possible.
- Wash your hands particularly well after using the toilet, changing diapers or coming into contact with animals.
- Blow your nose with a disposable handkerchief and then throw it away.
- Cough and sneeze into your sleeve and not into your hand.
- Ventilate regularly, because the number of pathogens can increase in closed rooms.
- Do not use any unused towels, washcloths or toothbrushes.
- Thoroughly clean raw fruits and vegetables before consuming them.
- After processing raw meat, be sure to clean the cutting boards and knives thoroughly to prevent other food from coming into contact with any bacteria.
- Wash your laundry regularly at 60 ° C, as most pathogens will not survive.
- Make sure you and your family are fully vaccinated. Do not forget to regularly refresh certain vaccinations.