Today, antibiotics are one of the most important groups of drugs used in the fight against bacterial infections in primary health care, in dental offices, in surgical treatment of wounds, as well as in complicated nosocomial infections. Thus, in modern medicine, the antibiotic takes the place of the most commonly prescribed and used drug.
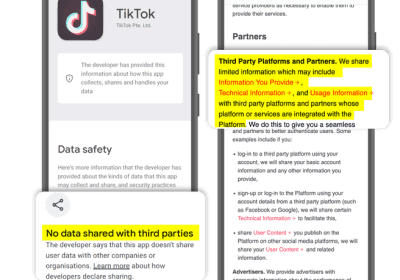
However, excessive enthusiasm for the effects of antibiotic therapy and their uncritical use leads to a new, very serious problem – resistance and insensitivity of microorganisms to antibiotics , which in turn leads to lower applicability, higher costs of treatment, and increased allergic reactions. and side effects. Here are some simple reasons and rules why, when and how to use antibiotics.
1. An antibiotic has no effect on viruses
The use of antibiotics in viral or fungal infections is wrong. The drug has the ability to slow down or kill only bacterial strains, but has no effect on the virus and its DNA / RNA. For example, it does not help with the common cold, which is of unknown origin, and occurs in the winter months when it is the season of infections and colds. It is almost always caused by viruses, but we often witness the administration of antibiotic therapy that has absolutely no effect on improving health. Not every fever, nasal congestion, sore throat or headache is an indication for an antibiotic.
 2. Always take the full dose prescribed by your doctor
2. Always take the full dose prescribed by your doctor
Consistent adherence to the prescribed dose and duration is of the utmost importance for the success of antibiotic therapy. Patients often dare to discontinue prescribed antibiotic therapy on their own, claiming that they feel healthy and have no additional need. Of course this is a big mistake and in this way the bacteria are given a great opportunity, which until then have been completely destroyed, to regenerate, relapse and make an infectious relapse (recurrence), while gaining resistance to the use of the same antibiotic. . Antibiotic resistance is a serious and major problem today.
3. Excessive use of antibiotics causes side effects
Conversely, due to the shortening of the prescribed therapy, the use of one or more types of antibiotics in large doses is excessive and often leads to side effects and adverse effects. They create additional problems for the patient. They usually have a negative effect on the intestinal flora and lead to diarrhea. Changes in the vaginal flora are also common in women, leading to excessive growth of the fungus Candida and causing a vaginal infection – candidiasis.
What may be more worrying than this type of antibiotic use is the growing incidence of allergic reactions. They are usually minor, in the form of: redness, itching, fever and headache. But sometimes they are more severe and lead to a life-threatening reaction to anaphylactic shock.
 4. Antibiotics and alcohol – of course you can NOT
4. Antibiotics and alcohol – of course you can NOT
Numerous studies and scientific studies on this topic certainly do not go in favor of those patients who receive antibiotic therapy and are lovers of the “good” glass of alcohol. When using alcohol and antibiotics, due to the “mutual interest” of the alcohol component and the active component of the antibiotic, the drug is canceled and its ineffectiveness is completely eliminated . This certainly leads to relapse or exacerbation of the disease. This is the case with most commonly used antimicrobials. It is therefore advisable for the patient to refrain from using alcohol during antibiotic therapy.
5. Always consult a doctor!
The decision to self-medicate without a doctor’s advice is the reason why many further problems arise. At the same time, this is the most common mistake that patients make. As easy and simple as prescribing an antibiotic may seem, misusing it can do more harm than good to the patient. It is very important to make a good diagnosis, to find the cause (whenever possible), to determine the severity of the disease, to know the patient himself (age, sex), as well as his medical history, all in order to prescribing the right antimicrobial drug. The drug should have the best positive effects, while minimizing the negative ones in the prevention or treatment of a certain disease and all that should be accompanied by the optimal price and quality of the same.